What is Problem-Solving in Nursing? (With Examples, Importance, & Tips to Improve)

Whether you have been a nurse for many years or you are just beginning your nursing career, chances are, you know that problem-solving skills are essential to your success. With all the skills you are expected to develop and hone as a nurse, you may wonder, “Exactly what is problem solving in nursing?” or “Why is it so important?” In this article, I will share some insight into problem-solving in nursing from my experience as a nurse. I will also tell you why I believe problem-solving skills are important and share some tips on how to improve your problem-solving skills.

What Exactly is Problem-Solving in Nursing?
5 reasons why problem-solving is important in nursing, reason #1: good problem-solving skills reflect effective clinical judgement and critical thinking skills, reason #2: improved patient outcomes, reason #3: problem-solving skills are essential for interdisciplinary collaboration, reason #4: problem-solving skills help promote preventative care measures, reason #5: fosters opportunities for improvement, 5 steps to effective problem-solving in nursing, step #1: gather information (assessment), step #2: identify the problem (diagnosis), step #3: collaborate with your team (planning), step #4: putting your plan into action (implementation), step #5: decide if your plan was effective (evaluation), what are the most common examples of problem-solving in nursing, example #1: what to do when a medication error occurs, how to solve:, example #2: delegating tasks when shifts are short-staffed, example #3: resolving conflicts between team members, example #4: dealing with communication barriers/lack of communication, example #5: lack of essential supplies, example #6: prioritizing care to facilitate time management, example #7: preventing ethical dilemmas from hindering patient care, example #8: finding ways to reduce risks to patient safety, bonus 7 tips to improve your problem-solving skills in nursing, tip #1: enhance your clinical knowledge by becoming a lifelong learner, tip #2: practice effective communication, tip #3: encourage creative thinking and team participation, tip #4: be open-minded, tip #5: utilize your critical thinking skills, tip #6: use evidence-based practices to guide decision-making, tip #7: set a good example for other nurses to follow, my final thoughts, list of sources used for this article.

- LOGIN / FREE TRIAL

‘Let’s celebrate those who have a phenomenal impact on nursing’
STEVE FORD, EDITOR
- Assessment skills
- Children’s nursing
- Hospital nursing
- You are here: Archive
Thinking your way to successful problem-solving
13 September, 2001 By NT Contributor
VOL: 97, ISSUE: 37, PAGE NO: 36
Jacqueline Wheeler, DMS, MSc, RGN, is a lecturer at Buckinghamshire Chilterns University College
Problems - some people like them, some do not think they have any, while others shy away from them as if they were the plague. Opportunities, in the form of problems, are part of your life.
The most difficult decision is deciding to tackle a problem and implement a solution, especially as it is sometimes easier to ignore its existence. Problem-solving takes time and effort, but once a problem has been addressed the nurse can feel satisfied that the issue has been resolved and is therefore less likely to re-emerge.
Nurses make clinical decisions using two different approaches. The first is the rationalist approach, which involves an analysis of a situation so that subsequent actions are rational, logical and based on knowledge and judgement. The second approach is based on a phenomenological perspective, where a fluid, flexible and dynamic approach to decision-making is required, such as when dealing with an acutely ill patient.
Types of problems
Problems come in different guises and the solver can perceive them either as a challenge or a threat. One of the most common types of problem is when the unexpected happens. As a nurse you plan and implement care for a patient based on your knowledge and experience, only to find that the patient’s reaction is totally different from that expected but without any apparent reason.
Another type of problem is an assignment where others set a goal or task. Throughout your working life you will be required to undertake duties on behalf of other people. For some this is difficult as they feel unable to control their workload. Others see it as an opportunity to develop new skills or take on additional responsibilities. Opportunities can be perceived as problems by those who fear failure.
A third type of problem is when a dilemma arises. This is when it is difficult to choose the best solution to a problem because the nurse is confronted with something that challenges his or her personal and/or professional values.
Diagnosing problems
The sooner a problem is identified and solutions devised, the better for all involved. So try to anticipate or identify problems when they occur through continuously monitoring staff performance and patient outcomes.
Listening to and observing junior staff will help you to detect work or organisational concerns, because when there are problems staff are likely to behave in an unusual or inconsistent manner.
Initial analysis
Remember that people view things differently, so what you perceive as a problem may not be one to anyone else. So before you begin thinking about what to do - whether to keep it under surveillance, contain it or find a solution - you should undertake an initial analysis. This will help you to understand the problem more clearly.
An analysis will also enable you to prioritise its importance in relation to other problems as problems do not occur one at a time.
Routine problems often need little clarification, so an initial analysis is recommended for non-routine problems only. Even then, not all problems justify the same degree of analysis. But where it is appropriate, an initial analysis will provide a basis from which to generate solutions.
Perception is also important when dealing with patients’ problems. For example, if a patient gives up reading because he or she cannot hold the book (objective), the nurse may assume it is because the patient has lost interest (subjective, one’s own view).
Generating solutions
It is essential for the problem-solver to remember that, where possible, solutions must come from those connected with the problem. If it is to be resolved, agreement must be owned by those involved as they are probably the best and only people who can resolve their differences. The manager should never feel that he or she must be on hand to deal with all disputes.
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993).
Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem. An effective tool for assisting in this process is the technique of lateral thinking, which is based largely on the work of Edward de Bono, who regards thinking as a skill.
There are several ways to encourage creative decision-making. One method that works best for specific or simple problems is brainstorming. If the ground rules of confidentiality and being non-judgemental are applied, it will produce a free flow of ideas generated without fear of criticism (Rawlinson, 1986).
Time constraints and staff availability may make it difficult for all those involved in a problem to meet. In such cases an adaptation of brainstorming - where a blank piece of paper is given to those involved and each writes down four solutions to the problem - may be the answer. A similar technique is the collective notebook, where people are asked to record their thoughts and ideas about a problem for a specified period.
An alternative is where one person writes down a list of solutions in order of priority, which is then added to by others. This helps to prioritise the ideas generated. All these methods produce data that can then be analysed by the problem-solver.
When the problem affects people in different geographical areas, solutions can be generated by obtaining the opinion of experts through the use of a questionnaire, which is known as the Delphi technique (McKenna, 1994).
When an apparently insurmountable problem presents itself, it is often useful to divide it into smaller pieces. This is known as convergent thinking. Using divergent thinking - where you consider a problem in different ways to expand your view - may also help.
A final alternative is the stepladder technique, which is time-consuming but effective if the issue is stirring up strong feelings. This requires the people involved in the problem to be organised into groups. First, two people try to solve the problem, then a third member is drawn in, to whom the solution reached by the first two is presented. All three then try to agree a solution. More people are added to the group, if necessary, in a similar way, until there is agreement of all involved. Provided the individuals are motivated to solve the problem, this technique creates ownership and commitment to implementing the agreed solution.
Analytical thinking, which follows a logical process of eliminating ideas, will enable you to narrow the range down to one feasible solution.
Although someone has to make the ultimate decision on which solution to implement, there are advantages to group decision-making: a greater number of possible solutions are generated and conflicts are resolved, resulting in decisions being reached through rational discussion.
This does, however, require the group to be functioning well or the individuals involved may feel inhibited in contributing to the decision-making. One individual may dominate the group or competition between individuals may result in the need to win taking precedence over deciding on an agreed practical solution.
As nursing becomes less bureaucratic individuals are being encouraged to put forward their own ideas, but social pressures to conform may inhibit the group. We do not solve problems and make decisions in isolation, but are influenced by the environment in which we work and the role we fulfil in that environment. If group members lack commitment and/or motivation, they may accept the first solution and pay little attention to other solutions offered.
Making a decision
There are three types of decision-making environments: certain, risk and uncertain. The certain environment, where we have sufficient information to allow us to select the best solution, is the most comfortable within which to make a decision, but it is the least often encountered.
We usually encounter the risk environment, where we lack complete certainty about the outcomes of various courses of action.
Finally, the uncertain environment is the least comfortable within which to make decisions as we are almost forced to do this blind. We are unable to forecast the possible outcomes of alternative courses of action and, therefore, have to rely heavily on creative intuition and the educated guess.
Taking this into consideration, you should not contemplate making a decision until you have all the information needed. Before you make your decision, remind yourself of the objective, reassess the priorities, consider the options and weigh up the strengths, weaknesses, opportunities and threats of each solution.
An alternative is to use the method that Thomas Edison used to solve the problem of the electric light bulb. Simply focus on your problem as you drift off to sleep, and when you wake up your subconscious mind will have presented you with the answer. But bear in mind that this is not a scientific way of solving problems - your subconscious can be unreliable.
If you are not sure about your decision, test the solution out on others who do not own the problem but may have encountered a similar dilemma. Once you have made your choice stick to it, or you may find it difficult to implement because those involved will never be sure which solution is current. They will also be reluctant to become involved in any future decision-making because of your uncertainty.
The next step is to ensure that all the people involved know what decision has been made. Where possible, brief the group and follow this up with written communication to ensure everyone knows what is expected of them. You may need to sell the decision to some, especially if they were not involved in the decision-making process or the solution chosen is not theirs.
Implementing the solution
Finally, to ensure the solution is implemented, check that the people involved know who is to do what, by when and that it has happened. Review the results of implementing your solution (see Box) and praise and thank all those involved.
- Part 1 of this series was published in last week’s issue: Wheeler, J. (2001) How to delegate your way to a better working life. Nursing Times; 97: 36, 34-35.
Next week. Part three: a step-by-step guide to effective report writing.
- Add to Bookmarks
- September 1,2024 | ISSN 1940-6967
- American Society of Registered Nurses ®

- OUR JOURNALS
- MEMBERSHIP BENEFITS

Featured Sponsors

- 8 Crucial Skills Every Nurse Should Master
By Staff
Mastering a set of core skills can help nurses navigate the complexities of their daily responsibilities. Whether it's communicating effectively with patients, thinking critically in high-pressure situations, or managing time efficiently, these skills lay the foundation for success in nursing.
Nursing is a demanding yet rewarding profession that requires a combination of skills, compassion, and dedication.
As healthcare continues to evolve, nurses play a crucial role in providing high-quality patient care. In order to excel in this field, it's not just about having a caring attitude but also about mastering essential skills that make a real difference in patient outcomes.
1. Upgrading Training & Education
Continuous learning is essential for nurses who want to keep their skills sharp and stay current in their field. Upgrading training and education can involve pursuing advanced certifications, attending workshops, or enrolling in education programs.
This commitment to learning not only enhances a nurse's knowledge but also opens up new opportunities for career advancement. By focusing on ongoing education, nurses can keep up with the latest medical advancements, technologies, and best practices. This not only benefits their careers but also improves the quality of care they provide to patients.
Life long learning is a key component of being a successful nurse, as it helps them remain competent and confident in their roles.
2. Online RN nursing programs
These programs offer a flexible, fully online format that allows working nurses to build on their existing knowledge and skills while gaining advanced training in leadership, evidence-based practice, and community health.

Clinical Competence
Clinical competence is at the heart of nursing. It involves having a strong grasp of medical knowledge, procedures, and patient care techniques. Nurses must be well-versed in various clinical tasks, from administering medications to monitoring vital signs and recognizing changes in a patient's condition. Being competent in these areas helps nurses deliver safe and effective care, which is crucial for patient recovery.
To build clinical competence, nurses should commit to continuous learning and practice. This can include attending workshops, participating in training sessions, or simply staying updated with the latest medical guidelines.
A competent nurse can confidently perform their duties, which boosts their confidence and earns the trust of patients and colleagues alike.
3. Effective Communication
Effective communication is essential for nurses as it directly impacts patient care and outcomes. Nurses need to communicate clearly with patients, their families, and the healthcare team.
Good communication helps to understand patient needs, provide clear instructions, and convey important information accurately.
Practicing active listening is a key part of effective communication. Nurses should take the time to listen to their patients concerns, answer questions, and provide reassurance. Simple gestures like maintaining eye contact and using a calm tone can also make a big difference in making patients feel heard and cared for.
4. Critical Thinking & Problem Solving
Critical thinking and problem-solving are skills that every nurse should develop early in their career. Nurses often face situations where they need to make quick decisions that can affect patient outcomes.
Having strong critical thinking skills allows them to assess situations accurately, identify potential problems, and choose the best course of action.

Problem-solving goes hand in hand with critical thinking. It's about finding practical solutions to challenges, whether it's managing a sudden change in a patient's condition or figuring out the best way to deliver care with limited resources. These skills can be sharpened through experience, reflection, and continuous learning.
5. Time Management & Organization
Time management and organization are crucial in nursing, where every second counts. Nurses juggle multiple tasks, such as administering medications, attending to patients, and coordinating with other healthcare professionals.
Good time management helps them prioritize these tasks effectively, reducing stress and improving the quality of care.
Being organized also plays a big role in managing time well. Simple strategies like creating checklists, using reminders, and planning the day ahead can help nurses stay on track. When nurses manage their time efficiently, they can attend to more patients, complete their tasks with fewer errors, and maintain a better work-life balance.
6. Emotional Intelligence
Emotional intelligence is the ability to understand and manage one's emotions while also being aware of others emotions. For nurses, this skill is vital as they deal with patients in various emotional states, from anxiety to grief. By developing emotional intelligence, nurses can respond more empathetically and provide support to patients who are going through difficult times.
Emotional intelligence also helps in managing stress and maintaining a positive attitude in challenging situations.
Nurses with high emotional intelligence can navigate their emotions better, leading to improved interactions with patients and a more harmonious work environment. Developing this skill involves being mindful of one's emotions, practicing empathy, and learning how to respond to others with compassion.
7. Teamwork & Collaboration

Teamwork and collaboration are at the heart of nursing because healthcare is a team effort. Nurses work closely with doctors, therapists, and other healthcare professionals to provide comprehensive care.
Being a good team player means communicating effectively, supporting colleagues, and contributing to a positive work environment.
Collaboration also involves sharing information and working together to solve problems. Nurses who excel at teamwork are not only good at their own jobs but also help their teams function better. This leads to improved patient outcomes and a more efficient healthcare system overall.
Building teamwork skills can be as simple as being approachable, respectful, and willing to lend a hand when needed.
8. Patient Advocacy
Patient advocacy is about standing up for patients needs and rights. Advocating for patients involves listening to them, respecting their wishes, and communicating their needs to the rest of the healthcare team.
Nurses should be prepared to speak up if they feel that a patient is not receiving the care they deserve or if they notice something that needs attention. This can be challenging, but it is an important part of the nurse's role. By being a strong advocate, nurses help patients navigate the healthcare system and receive the best possible care.
Mastering these essential skills can significantly impact a nurse's ability to deliver quality care and succeed in their profession. By continuously working on these skills, nurses can improve their performance, provide better patient care, and advance their careers.
As healthcare continues to evolve, these skills will help nurses meet new challenges and provide the best possible care to their patients. Developing these skills is an ongoing process, but the rewards are well worth the effort.

Articles in this issue:
- Nurse Quits Job, Switches Careers, Triples Her Income: 'Best Decision'
- This Is How Pandemics Start: A Frightening H5N1 Development
- Report: High Lead Levels Found In Cinnamon, Spice Blends From 12 Brands
- How Your Dog Changes Your Brain
- UTIs Are Rising Fast—And The Cause Could Be In Your Refrigerator
- Ozempic Curbs Hunger – And Not Just for Food

Journal of Nursing Sign Up
Get the journal of nursing delivered to your inbox., in this issue.
- December 1, 2024
- November 1, 2024
- October 1, 2024
- September 1, 2024
- August 1, 2024
- July 1, 2024
- June 1 , 2024
- May 1, 2024
- April 1, 2024
- March 1, 2024
- February 1, 2024
- January 1, 2024
- December 1, 2023
- November 1, 2023
- October 1, 2023
- September 1, 2023
- August 1, 2023
- July 1, 2023
- June 1, 2023
Masthead Editor-in Chief: Kirsten Nicole Editorial Staff: Kirsten Nicole Stan Kenyon Robyn Bowman Kimberly McNabb Lisa Gordon Stephanie Robinson
Contributors: Kirsten Nicole Stan Kenyon Liz Di Bernardo Cris Lobato Elisa Howard Susan Cramer

Sign Up for the Journal of Nursing.
Leave a comment.
Please keep in mind that all comments are moderated. Please do not use a spam keyword or a domain as your name, or else it will be deleted. Let's have a personal and meaningful conversation instead. Thanks for your comments!
Your name *
Your email *
Your message *

- Privacy Policy
- Unsubscribe
Problem Solving Skills - Nursing Science
Why are problem solving skills crucial in nursing, what are the key problem solving steps in nursing, how do nurses gather data for problem solving, what role does critical thinking play in nursing, how do nurses develop effective care plans, how do nurses implement and evaluate interventions, what tools and resources can assist in problem solving, how can teamwork enhance problem solving, what challenges do nurses face in problem solving, how can nurses improve their problem solving skills, relevant publications.
Issue Release: 2024
Partnered Content Networks

Relevant Topics
- AI in Healthcare
- Anomaly Detection
- antimicrobial resistance
- anxiety disorders
- anxiety symptoms physical
- Artificial Intelligence
- Behavioral Disturbances
- bioimpedance
- burnout prevention
- Care Providers
- Caregiver Support
- Clinical Decision-Making
- Delirium management
- Delirium prevention ICU
- disaster response
- electronic health records
- Emergency preparedness
- flexible electronics
- Gaussian Mixture Models
- Hand Hygiene
- Health Workforce
- healthcare management
- Healthcare Workers
- Healthcare-associated infections
- holistic nursing care
- hypertensive patients
- ICU delirium
- ICU delirium care
- ICU delirium treatment
- ICU patient delirium
- infection control
- Infection Prevention
- Integrated Care
- Medical Practices
- mental disorders
- Mental Health
- Mental Health Screening
- Musculoskeletal Complaints
- near-field communication
- Nurse caring
- nurse caring behaviors
- nurse staffing
- nurse well-being
- Nurses in ICU
- Nursing Care
- Nursing Education
- nursing informatics
- nursing management
- nursing practice
- Nursing strategies for delirium Critical care delirium
- Paternalism
- Patient Monitoring
- patient outcomes
- patient safety
- patient satisfaction
- Patient-Centered Care
- patient-generated health data
- Pediatric Care
- Personalized Medicine
- pharmacological strategies
- physical activity and mental health
- physical health and mental health
- physical symptoms of mental illness
- physiological care
- precision medicine
- Predictive Analytics
- Protective Empowering
- psychiatric disorder
- Psychiatric Disorders
- Psychiatric Nursing
- Psychological
- psychological care
- Psychological Emotional
- Psychometric
- public health
- Quality in health care
- real-time monitoring
- Recurrent Autoencoders
- Relational Autonomy
- Remote Patient Monitoring
- Rheumatologists
- Rheumatology
- role of nurse
- Role of nurses in delirium
- smart wound dressings
- sociocultural care
- spiritual care
- targeted treatment
- technology in healthcare
- telemedicine
- Thematic Analysis
- Unsupervised Learning
- Variational Autoencoders
- Wound assessment
- Wound healing
- Wound infection control
Subscribe to our Newsletter
Stay updated with our latest news and offers related to Nursing.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Communication Skills, Problem-Solving Ability, Understanding of Patients’ Conditions, and Nurse’s Perception of Professionalism among Clinical Nurses: A Structural Equation Model Analysis
Ae young kim.
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected] ; Tel.: +82-10-3372-5920; Fax: +82-2-824-7961
Received 2020 Jun 18; Accepted 2020 Jul 5; Issue date 2020 Jul.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/ ).
This study was intended to confirm the structural relationship between clinical nurse communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Due to changes in the healthcare environment, it is becoming difficult to meet the needs of patients, and it is becoming very important to improve the ability to perform professional nursing jobs to meet expectations. In this study method, structural model analysis was applied to identify factors influencing the perception of professionalism in nurses. The subjects of this study were 171 nurses working at general hospitals in city of Se, Ga, and Geu. Data analysis included frequency analysis, identification factor analysis, reliability analysis, measurement model analysis, model fit, and intervention effects. In the results of the study, nurse’s perception of professionalism was influenced by factors of communication skills and understanding of the patient’s condition, but not by their ability to solve problems. Understanding of patient’s condition had a mediating effect on communication skills and nursing awareness. Communication skills and understanding of the patient’s condition greatly influenced the nurse’s perception of professionalism. To improve the professionalism of clinical nurses, nursing managers need to emphasize communication skills and understanding of the patient’s condition. The purpose of this study was to provide a rationale for developing a program to improve job skills by strengthening the awareness of professional positions of clinical nurses to develop nursing quality of community.
Keywords: communication, clinical nurse, perception of professionalism, patient’s condition, structural equation model
1. Introduction
Changes in the environment related to climate and pollution are causing health problems and various diseases such as respiratory and circulatory problems, metabolic disorders, and chronic diseases. Moreover, access to modern healthcare facilities has created greater expectations among patients receiving personalized healthcare and high-quality healthcare. As the difficulty of satisfying the demands of patients increases, enhancing nursing capabilities has become increasingly important [ 1 ]. To improve this, hospitals are making efforts to change the internal and external environments so as to increase the number of nurses, reduce the length of hospital stays, and enable efficient nursing practice. Despite these efforts, the workloads of nurses and the demand for clinical nurses are continuously increasing [ 2 , 3 ]. As a result, nurses are developing negative attitudes and prejudices toward patients, as well as negative perceptions of professionalism. To address this, the cultivation and strengthening of nursing professionals’ capabilities is essential.
Nurses’ perception of professionalism is an important element influencing their ability to perform independent nursing, and a good perception of their profession results in a positive approach to solving patients’ problems [ 4 , 5 ]. In addition, the characteristics and abilities of individual nurses can influence the level of care and enable them to understand patients, solve problems, and provide holistic care, which is the ultimate goal of the nursing process [ 6 , 7 ]. Thus, patients expect nurses to not only have medical knowledge of the disease but to also be able to comprehensively assess the patient’s problems and be independent and creative in nursing [ 8 ]. This attitude can have a major impact on the quality of nursing services and can inspire pride in the nursing occupation and professional achievement. These findings can also be used by nurses to prevent burnout and maintain professionalism [ 9 , 10 ].
To respond to the increasing demands for diverse qualitative and quantitative nursing services and to strengthen the capabilities of nursing professionals, efforts have been made to move nursing education toward scientific and creative education. However, in point-of-care environments, not only are nurses prevented from making independent decisions regarding nursing, but also the diverse personal capabilities necessary for such independent behavior are not sufficiently developed [ 11 ]. Therefore, it is important to enhance clinical nurses’ perceptions of the nursing profession; maintain a balance of nursing capabilities; provide novel, high-quality nursing services; and identify assistive nursing education methods and obstructive environmental factors [ 10 ].
Communication skills involve a person’s ability to accurately understand (through both verbal and non-verbal indications) another person, and sufficiently deliver what the person desires [ 12 , 13 ]. Good communication skills are a primary requirement for providing professional nursing services because they enable an in-depth understanding of patients, solving of complicated problems, and reasonable and logical analysis of situations [ 14 , 15 , 16 ]. When effective communication takes place, nurses’ problem-solving abilities and perceived professionalism strengthen [ 17 , 18 ].
According to Park [ 19 ], nurses have difficulties in interpersonal relationships when social tension and interaction skills are low and communication is poor. In addition, these factors are negatively affected not only in the work of the nurse but also in the perception of the profession. Communication skills are associated with both the formation of relationships with patients and the ability to perform holistic nursing [ 20 ]. In order to improve and develop the overall nursing function of a clinical nurse like this, it is important to complement the relevant integrated nursing abilities [ 21 , 22 ].
Previous studies have investigated the importance of communication skills for nurses, and the relationships between nurses’ problem-solving ability and their understanding of the patients’ conditions. Nonetheless, data that can comprehensively explain the structural relationships between these qualities and how they affect the job perception of nurses remains insufficient.
Therefore, the present study aims to identify the structural model for the relationships between nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Additionally, the study provides basic data necessary for developing programs for improving nursing abilities.
The purpose of this study is to construct a theoretical model that explains the structural relationships among nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. In addition, the study aimed to verify this model using empirical data.
2. Materials and Methods
2.1. study design.
To create and analyze the structural model for clinical nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism, the theoretical relationships among the variables were developed based on related theories.
In this study, communication skills were set as the exogenous variables, whereas problem-solving ability, understanding of patients’ conditions, and perception of the nursing occupation were set as the endogenous variables. In addition, communication skills were set as the independent variables and nursing job perceptions as the dependent variable. This is because the ability of communication helps to maintain an intimate relationship with the patient and to assess the patient’s condition through each other’s relationship and to solve problems and develop correct understanding. Communication skills, problem-solving ability, and understanding of patients’ conditions were set as the parameters for determining causality. The research model is shown in Figure 1 .
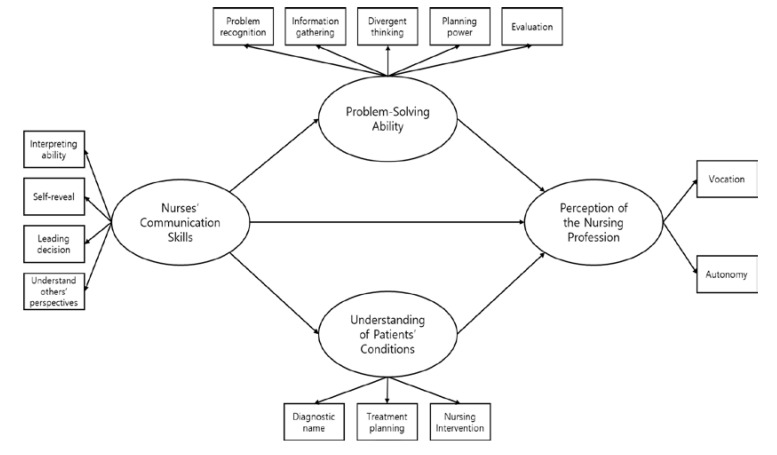
Study model.
2.2. Study Participants
The structural equation model has less than 12 measurement variables. The sample size usually requires 200 to 400 participants [ 23 ]. A total of 250 participants were selected for the study. In line with ethical standards and practices, participants received a full explanation on the purpose of the study. They were briefed that the information collected would be used for research purposes only. Furthermore, they were informed that they could withdraw from the study at any time.
2.3. Data Collection Method
Data collection for this study was performed by two researchers unrelated to the hospital from April 20 to May 1, 2019. A questionnaire was used to collect data from clinical nurses working in five hospitals in Seoul, Gyeonggi, and Gangwon provinces. Of the 250 questionnaires disseminated, we received 225 completed returns. However, 54 were considered inaccurate, inconsistent, or unsatisfactory for coding purposes. Thus, 171 fully completed valid questionnaires comprised the final dataset for analysis.
2.4. Research Instruments
2.4.1. communication skills.
In this study, the communication skill instrument developed by Lee and Jang [ 24 ] was used. Its contents were modified and supplemented to clearly understand the communication skills of nurses. Our questionnaire comprised 20 questions with five questions each concerning “interpretation ability,” “self-reveal,” “leading communication,” and “understanding others’ perspectives.” The answers were rated on a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” For this study, the Cronbach’s alpha value was 0.81.
2.4.2. Problem-Solving Ability
The tool developed by Lee [ 25 ] was used to measure the problem-solving ability of clinical nurses. The survey comprised 25 questions, with five questions each concerning “problem recognition,” “information-gathering,” “divergent thinking,” “planning power,” and “evaluation.” Items were scored on a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” The internal consistency confidence value Cronbach’s alpha was 0.79.

2.4.3. Understanding Patients’ Condition
To measure nurses’ understanding of patients’ conditions, we developed 10 questions by revising and supplementing items from an existing understanding-measurement tool [ 26 ]. With a total of ten questions, we measured “diagnostic name,” “patient-treatment planning,” and “nursing intervention processes.” Items were scored using a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” The internal consistency confidence value Cronbach’s alpha was 0.81.
2.4.4. Nurse’s Perception of Professionalism
Nurse’s perception of professionalism was measured using a tool developed by revising the 25 questions created by Kang et al. [ 1 ]. With a total of ten questions, we measured “vocation” and “autonomy.” Items were scored using a five-point Likert scale. The internal consistency confidence value Cronbach’s alpha was 0.81.
2.5. Data Analysis
To identify the relationships among the set variables, the data were computed statistically using the program included in IBM SPSS 24.0 and AMOS 23.0. (IBM Corp., Armonk, NY, USA). The analysis methods were as follows:
Frequency analysis was conducted to identify the subjects’ demographic and general characteristics.
The reliability of the questionnaire was verified using Cronbach’s α coefficients.
Confirmatory factor analysis (CFA) was performed to verify the convergent validity of the selected measurement tool.
The normality of the data was determined through analyzing the skewness and kurtosis of the measurement variables.
The fitness of the model was verified using structural equation modeling (SEM).
Bootstrapping was utilized to verify the mediating effect in the set study model, as well as the mediating effects of the nurses’ problem-solving ability and understanding of patients’ conditions.
3.1. Demographic Characteristics
The demographic and general characteristics of the study subjects are shown in Table 1 . Overall, 71 respondents were aged 25–29 years (41.5%), representing the most numerous age group. University graduates comprised 113 (66.1%) of the sample, while 50 (29.2%) held graduate degrees, with eight (4.7%) holding master’s degrees. Fifty-three respondents (31.0%) had over seven years of clinical experience, 43 (25.1%) had two to three years of experience, 42 (24.6%) had four to six years of experience, and 33 (19.3%) had less than two years of experience. Additionally, 121 respondents (70.8%) worked at secondary hospitals, while 50 (29.2%) worked at tertiary hospitals; 159 respondents (93.0%) reported that they were general nurses.
Participants’ general characteristics ( N = 171, %).
3.2. Technical Metrics of the Measurement Variables
The multivariate normality of the findings related to the factors of the latent variables was verified through standard deviations, skewness, and kurtosis. The present study meets the criteria for the skewness and kurtosis values mentioned by Hu and Bentler [ 27 ].
All sub-factors of the latent variables secured normality.
In this study, a normal distribution was obtained for each of the four sub-factors of communication skills, five sub-factors of problem-solving ability, three sub-factors for understanding the patient’s condition, and two sub-factors of the nurse’s perception of professionalism as shown in Table 2 .
Technical metrics of the measurement variables ( N = 171).
3.3. Correlations between the Measured Variables
The correlations between the measurement variables were analyzed using Pearson’s product–moment correlation coefficient analysis ( Table 3 ). The correlations among all individual measurement variables were found to show a positive correlation.
Correlations between the observed variables.
3.4. Confirmatory Factor Analysis of the Measurement Model
This study examined how well the measurement variables represented the latent variables in the measurement model. Each set path coefficient was evaluated using non-standardization factors, standardization factors, and standard errors. The path coefficients refer to the factor loadings in CFA. The standardization factors of the individual paths were shown to be at least 0.50 (except for vocation: 0.36), and the critical ratio (CR) was at least 1.96. This indicated that the measurement tool had good convergent validity ( Table 4 ).
Confirmatory factor analysis of the measurement model.
*** p < 0.001; CR: critical ratio.
3.5. Verification of the Structural Model
The structural model for relationships among clinical nurses’ communication skills, problem-solving ability, understanding of patients’ condition, and nurse’s perception of professionalism that would be suitable for predicting the influencing relationships was verified. Since the fitness index of the modified model was shown to be higher than that of the initial model, the final model for this study was set as shown in Figure 2 .
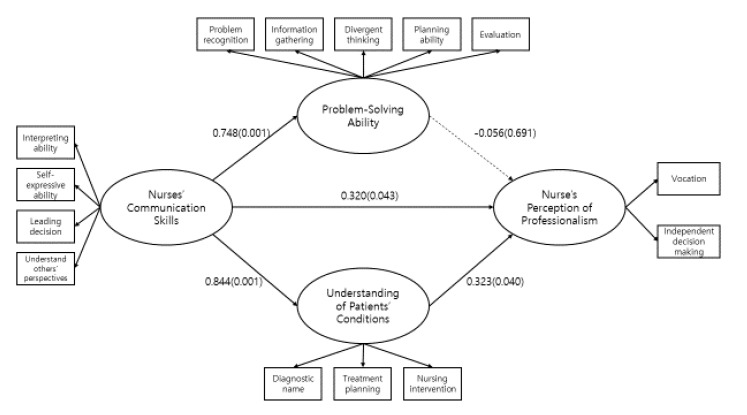
Final model. * χ 2 = 124.074 (df = 61, p <0.001), GFI(Goodness of Fit Index)= 0.90, RMSEA(Root Mean Square Error Approximation)=0.07, NFI(Normed Fit Index)=0.87, IFI(Incremental Fit Index)= 0.93, TLI(Tucker-Lewis Index)= 0.91, CFI(Comparative Fit Index)= 0.92.
3.6. Influencing Relationships between Variables of the Study Model
The standardization factors and CR values of the final model were examined to determine whether there were direct relationships between communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. The results are shown
For the relationship between communication ski in Table 5 .lls and problem-solving ability, the standardization factor was 0.85 and the CR value was 7.37; communication skills showed a statistically significant effect. Consequently. The relationship between communication skills and understanding of patients’ conditions also showed a statistically significant effect. Consequently, Hypothesis 1 was supported.
The relationships between the human effects of the measurement model.
* p < 0.05, *** p < 0.001; CR: critical ratio.
For the relationship between communication skills and nurse’s perception of professionalism, the standardization factor was 0.54, and the CR value was 2.02. Communication skills showed a statistically significant effect. Consequently. For the relationship between problem-solving ability and nurse’s perception of professionalism, the standardization factor was −0.056, and the CR value was −0.39. Problem-solving ability had no statistically significant effect. Consequently.
The relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism had a statistically significant effect. Consequently Figure 2 shows the influencing relationships between the study variables of the final study model, considering non-standardization and standardization factors of the relationships between the study variables.
3.7. Direct and Indirect Effects of the Variables
To grasp the significance of the mediating effect in the final study model, the direct and indirect effects of each variable were examined. To examine the mediating effect of the problem-solving ability and understanding of patients’ conditions variables, the bootstrapping method provided by the AMOS 23.0 program included in IBM was utilized. The results are shown in Table 6 .
Mediating effect analysis.
* p < 0.05, *** p < 0.001
The indirect effect of communication skills on nurse’s perception of professionalism through nurses’ understanding of patients’ conditions was statistically significant. That is, clinical nurses’ communication skills have an indirect positive effect on their nurse’s perception of professionalism, with nurses’ understanding of patients’ conditions acting as a parameter. We also found that the effect of communication skills on nurse’s perception of professionalism was statistically significant. Therefore, communication skills have a partially mediated effect on nurse’s perception of professionalism, with understanding of patients’ conditions acting as a parameter. However, communication skills were found to have no indirect positive effect on nurse’s perception of professionalism when problem-solving ability was set as a parameter.
4. Discussion
In this study, we developed and analyzed a hypothetical model regarding clinical nurses’ communication skills, problem-solving ability, and understanding of patients’ conditions, and how these factors influence their nurse’s perception of professionalism.
4.1. Effect of Communication Skills on Nurses’ Perception of Professionalism
Communication skills were found to have statistically significant effects on their relationship with nurses’ problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Nurses’ communication skills not only affected their problem-solving ability but also their understanding of patients’ conditions and nurse’s perception of professionalism. Good communication among nurses can reduce uncomfortable situations and improve interactions with patients, which can consequently enhance problem-solving [ 28 ]. Supporting our findings, Ancel [ 17 ] reported that communication skills afford the maintenance of amicable cooperative relationships with patients across diverse medical classes, thereby enhancing the efficiency of nursing-related problem-solving.
Nurses’ communication is also closely related to their understanding of patients’ conditions, particularly regarding the treatment processes. Nurses frequently experience difficulties as a result of poor communication with not only patients and their family members but also other medical personnel. Further, poor delivery of explanations and questions affects nurses’ understanding of patients’ situations and problems, and patients can also feel concern regarding whether nurses accurately understand their problems [ 29 ]. Nurses frequently experience psychological abuse when communicating with patients and develop stress or discomfort [ 30 ]; this can lead to distrustful relationships with and inhibited understanding of patients [ 31 , 32 ]. Vermeir et al. [ 18 ] reported that scientific approaches are required to understand patients in-depth. To accurately understand both oneself and others, the most important method is successful communication. Such findings support the present study’s indication that nurses’ communication is a basic means of solving nursing problems, with both actions being interrelated.
Our finding that nurses’ communication skills are structurally related to their nurse’s perception of professionalism supports the findings of many previous studies. Regarding nurse’s perception of professionalism, Adams et al. [ 33 ] as well as Lee and Kim [ 34 ] explained that a good perception leads to higher-level capabilities, fostering high-level nursing of patients and the development of autonomous vocation. The above studies reported that, since nurses’ communication skills are related to their nurse’s perception of professionalism, communication skills should be considered a predictor of success. Further, McGlynn et al. [ 35 ] recommended positively reinforcing communication skills to improve nurse’s perception of professionalism. This supports the findings of the present study, indicating that communication and nursing professional perception are interrelated.
Thus, communication skills are important for nursing patients. They enable nurses to accurately understand patients’ problems, serve (by forming patient trust) an important function in the process of administering nursing interventions, and positively affect nurses’ perception of their profession. As such, each concept is important. However, nurses working in the clinic are critically aware of their professionalism. In order to reinforce this, communication skills are required, and the emphasis is placed on strengthening the nurses’ ability to solve problems as well as assess and understand patients. As a result, communication skills play an important role in helping nurses understand patients’ problems accurately, build patient trust in nursing interventions, and create structural relationships that have a positive impact on the perception of nursing occupations. Therefore, efforts to improve nurses’ communication skills not only improve their problem-solving abilities and understanding of patients’ conditions but also improve their nurse’s perception of professionalism. To maintain the professionalism of nurses, “competency development programs” would be helpful, thereby emphasizing the need for their application in nursing colleges and clinical practice.
4.2. Relationship between Nurses’ Problem-Solving Ability and Nurse’s Perception of Professionalism
We found clinical nurses’ problem-solving ability to have no positive effect on their perception of professionalism. This contrasts with previous studies, which reported that problem-solving ability is helpful for such perception of professionalism [ 36 ]. We also found that problem-solving ability does not affect nursing professional perception through a mediating effect.
The present findings indicate that the distinctiveness of the fields of nursing should not be overlooked. In nursing organizations that have a culture of discouraging diversity, when negative results are obtained from attempts to solve nursing problems, confusion regarding the identity of nursing professionals means perception of the profession is not reinforced; in many cases, the opposite perception is formed. Furthermore, for those in lower-level positions, nurse’s perception of professionalism is thought to be low because they cannot voice their opinions and have difficulties such as excessive workloads. Although few previous studies have directly examined this, Vermeir et al. [ 18 ] explained that, as the role expectation for nurses increases, factors for job turnover increase as a result of a sense of confusion regarding the nurses’ role and increases in stress. These findings indicate that factors that degrade nurses’ problem-solving ability induce skepticism regarding nursing and possibly career change, thereby supporting the findings of this study.
However, in the present study, positive results with low levels of relevancy in the structural model but high correlations were found. It is expected that, if nurses’ environmental conditions are improved and their nursing capabilities are developed so that they can solve nursing problems with confidence, their nursing professional perception will improve.
4.3. Relationship between Nurses’ Understanding of Patients’ Conditions and Nurse’s Perception of Professionalism
Our findings indicated that the relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism was statistically significant. This supports Nilsson et al. [ 21 ] and Philip et al. [ 29 ], who reported that, in the fields of nursing, when patients accurately understand nurses’ instructions or explanations and health information, they can participate in, independently adjust, and engage in creative decision-making related to self-nursing.
McGlynn et al. [ 35 ] suggested that understanding patient problems is an important element in resolving negative situations; meanwhile, Heo and Lim [ 37 ] indicated that clinical nurses provide high-quality nursing services and develop self-efficacy when they apply professional knowledge and a desire to understand patients’ problems. These study findings accord with our own findings.
The aforementioned findings suggest that the development and application of programs that can enhance nurses’ understanding of patients’ conditions should be emphasized, and that studies of various patient types, the characteristics of patients by age group and hospital areas, as well as the introduction of simulation education programs to improve nurses’ understanding of patients’ conditions should be continuously implemented.
5. Conclusions
This study aimed to verify the structural relationships between clinical nurses’ communication skills and their problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. We also aimed to identify, through a structural model, the mediating effects of nurses’ problem-solving ability and understanding of patients’ conditions in the relationship between communication skills and nurse’s perception of professionalism.
The findings of this study are as follows (all significance levels = 0.05). In the relationship between communication skills and problem-solving ability, the value of the standardization factor was 0.85 and the CR value was 7.37, indicating that communication skills had a statistically significant effect. In the relationship between nurses’ communication skills and understanding of patients’ conditions, the value of the standardization factor was 0.61 and the CR value was 6.35, indicating that communication skills had a statistically significant effect. In the relationship between communication skills and nurse’s perception of professionalism, the value of the standardization factor was 0.54 and the CR value was 2.02, indicating that communication skills had a statistically significant effect. However, in the relationship between problem-solving ability and nurse’s perception of professionalism, the value of the standardization factor was −0.05 and the CR value was −0.39, indicating that problem-solving ability has no statistically significant effect. Finally, in the relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism, the value of the standardization factor was 0.56, and the CR value was 2.14, indicating that nurses’ understanding of patients’ conditions has a statistically significant effect.
There are some limitations to this study. First, as we only examined nurses at secondary and tertiary university hospitals, our findings may not be generalizable to all clinical nurses. Replication studies examining a range of levels of medical institutions and associated workers are necessary. Second, the structural relationship between problem-solving ability and the nurse’s perception of professionalism turned out to be insignificant or mediated. Subsequent studies on the various approaches to revisit this structural relationship should be performed. Third, theories should be systematically developed to establish the values of the nursing profession, and additional studies are necessary to explore other variables.
Acknowledgments
We would like to thank the staff nurses who participated in the survey and took the time to complete the initial assessment.
Author Contributions
Conceptualization, A.Y.K. and I.O.S.; methodology, A.Y.K.; software, I.O.S.; validation, A.Y.K. and I.O.S.; formal analysis, A.Y.K. and I.O.S.; investigation, A.Y.K.; resources, A.Y.K.; data curation, A.Y.K.; writing—original draft preparation, A.Y.K.; writing—review and editing, A.Y.K. and I.O.S.; visualization, A.Y.K. and I.O.S.; supervision, I.O.S.; project administration, I.O.S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
- 1. Kang J.W., Lee Y.N., Kang P. Nurses’ perceptions of the professionalism in comprehensive nursing care service wards. J. KSSSS. 2019;45:45–66. [ Google Scholar ]
- 2. Dean A.R., Beyer E., Carter K. Connecting a school of nursing and a professional nurse organization to promote concussion awareness. J. Emerg. Nurs. 2018;44:86–88. doi: 10.1016/j.jen.2017.10.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Durmaz Y.C., Serin E.K., Polat H.T. Determination of problem-solving and communication skills of nursing/midwifery students. Int. J. Caring Sci. 2018;11:1771–1777. [ Google Scholar ]
- 4. Kim H.J., Kim H.Y. Experience of job stress among nurses working in long-term care hospital: A phenomenological approach. Korean J. Adult Nurs. 2016;28:572–584. doi: 10.7475/kjan.2016.28.5.572. [ DOI ] [ Google Scholar ]
- 5. Ning S., Zhong H., Qiujie L. The impact of nurse empowerment on job satisfaction. J. Adv. Nurs. 2009;65:2642–2648. doi: 10.1111/j.1365-2648.2009.05133.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Niknam F., Khammarnia M., Zand F., Fallahnejad E., Sharifian R. Evaluating physicians and nurses’ satisfaction with computerized physician order entry system in Iran. J. Health Manag. Inform. 2018;5:51–56. [ Google Scholar ]
- 7. Oprescu F., McAllister M., Duncan D., Jones C. Professional development needs of nurse educators. An Australian case study. Nurs. Educ. Pract. 2017;27:165–168. doi: 10.1016/j.nepr.2017.07.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Bang M., Sim S. Relationship among empathy ability, creativity confluence competency and problem-solving ability in nursing students. Indian J. Public Health Res. Dev. 2018;9:939–944. doi: 10.5958/0976-5506.2018.00851.3. [ DOI ] [ Google Scholar ]
- 9. Kwak S.Y., Kim Y.S., Lee K.J., Kim M. Influence of nursing informatics competencies and problem-solving ability on nursing performance ability among clinical nurses. J. Korean Acad. Nurs. Adm. 2017;23:146. doi: 10.5977/jkasne.2017.23.2.146. [ DOI ] [ Google Scholar ]
- 10. Morita K., Matsui H., Yamana H., Fushimi K., Imamura T., Yasunaga Y. Association between advanced practice nursing and 30-day mortality in mechanically ventilated critically ill patients: A retrospective cohort study. J. Crit. Care. 2017;41:209–215. doi: 10.1016/j.jcrc.2017.05.025. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Hoeksel R., Eddy L., Dekker L., Doutrich D. Becoming a transformative nurse educator: Finding safety and authenticity. Int. J. Nurs. Educ. Scholarsh. 2019;1:1–8. doi: 10.1515/ijnes-2018-0073. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Ceravolo D.J., Schwartz D.G., Foltz K.M., Castner J. Strengthening communication to overcome lateral violence. J. Nurs. Manag. 2012;20:599–606. doi: 10.1111/j.1365-2834.2012.01402.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Boyd C., Dare J. Communication Skills for Nurses. John Wiley & Sons, Inc.; New York, NY, USA: 2015. [ Google Scholar ]
- 14. Curtis K., Tzannes A., Rudge T. How to talk to doctors—A guide for effective communication. Int. Nurs. Rev. 2011;58:13–20. doi: 10.1111/j.1466-7657.2010.00847.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Clements A., Curtis K., Horvat L., Shaban R.Z. The effect of a nurse team leader on communication and leadership in major trauma resuscitation. Int. Emerg. Nurs. 2015;23:3–7. doi: 10.1016/j.ienj.2014.04.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Pangh B., Jouybari L., Vakili M.A., Sanagoo A., Torik A. The effect of reflection on nurse-patient communication skills in emergency medical centers. J. Caring Sci. 2019;8:75–81. doi: 10.15171/jcs.2019.011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Ancel G. Problem-solving training: Effects on the problem-solving skills and self-efficacy of nursing students. Eurasian J. Educ. Res. 2016;64:231–246. doi: 10.14689/ejer.2016.64.13. [ DOI ] [ Google Scholar ]
- 18. Vermeir P., Blot S., Degroote S., Vandijck D., Mariman A., Vanacker T., Peleman R., Verhaeghe R., Vogelaers D. Communication satisfaction and job satisfaction among critical care nurses and their impact on burnout and intention to leave: A questionnaire study. Intensive Crit. Care Nurs. 2018;48:21–27. doi: 10.1016/j.iccn.2018.07.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Park S.J. Effects of video debriefing on self-efficacy, problem solving ability and learning satisfaction of nursing students in ICU-based simulation education. J. Korean Soc. Simul. Nurs. 2017;5:31–40. [ Google Scholar ]
- 20. Hopkinson S.G., Oblea P., Napier C., Lasiowski J., Trego L.L. Identifying the constructs of empowering nurse leader communication through an instrument development process. J. Nurs. Manag. 2019;27:722–731. doi: 10.1111/jonm.12729. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Nilsson J., Engstrom M., Florin J., Gardulf A., Carlsson M. A short version of the nurse professional competence scale for measuring nurses’ self-reported competence. Nurse Educ. Today. 2018;71:233–239. doi: 10.1016/j.nedt.2018.09.028. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Hwang H.J., Lim J.H. The effects of nursing professional intuition and self-leadership on organizational commitment in clinical nurses. JLCC. 2018;18:1155–1171. doi: 10.22251/jlcci.2018.18.24.1155. [ DOI ] [ Google Scholar ]
- 23. Bae B.R. Structural Equation Modeling with AMOS 7: Principles and Practice. Choungram Books; Seoul, Korea: 2007. [ Google Scholar ]
- 24. Lee J.A., Jang M.H. The influences of critical thinking ability, communication skills, leadership, and professionalism on clinical practice ability in nursing students. J. East.West. Nurs. Res. 2017;25:124–133. doi: 10.14370/jewnr.2017.23.2.124. [ DOI ] [ Google Scholar ]
- 25. Lee S.J. Ph.D. Thesis. Chon-nam National University; Gwangju, Korea: 2009. The Effects of Action Learning Program on Nurses’ Problem Solving and Communication Skills. [ Google Scholar ]
- 26. Paek K.S. Impact of health literacy on adherence to self-care behavior among the elderly with hypertension in a community. Crisionomy (KRCEM) 2015;8:157–174. [ Google Scholar ]
- 27. Hu L.Z., Bentler P.M. Cut off criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6:1–55. doi: 10.1080/10705519909540118. [ DOI ] [ Google Scholar ]
- 28. Kim H.S., Han S.J. The survey on the influence of clinical nurse’s critical thinking disposition, problem-solving skill and self-efficacy on patients’ safety competencies. J. Korea Acad. Ind. Coop. Soc. 2016;17:598–608. doi: 10.5762/KAIS.2016.17.6.598. [ DOI ] [ Google Scholar ]
- 29. Philip S., Woodward-Kron R., Manias E., Noronha M. Overseas qualified nurses’ (OQNs) perspectives and experiences of intra professional and nurse-patient communication through a community of practice. Collegian. 2019;26:86–94. doi: 10.1016/j.colegn.2018.04.002. [ DOI ] [ Google Scholar ]
- 30. Nikmanesh P., Mohammedzadeh B., Nobakht S., Yusefi A.R. Nurses communication skills training and its effect on patients’ satisfaction in teaching hospitals of Shiraz University of Medical Sciences. J. Maz. Univ. Med. Sci. 2018;6:22–29. doi: 10.18502/jhs.v6i4.201. [ DOI ] [ Google Scholar ]
- 31. Kim S.H., Lee M.A. Effects of emotional labor and communication competence on turnover intention in nurses. J. Korean Acad. Nurs. Adm. 2014;20:332–341. doi: 10.11111/jkana.2014.20.3.332. [ DOI ] [ Google Scholar ]
- 32. Kim S.M., Park M.J., Yang Y.K. Effects on problem solving ability and learning satisfaction of nursing students of receiving a teaching method using standardized patients—Blood transfusion. J. Korean Acad. Nurs. Adm. 2015;22:406–415. doi: 10.7739/jkafn.2015.22.4.406. [ DOI ] [ Google Scholar ]
- 33. Adams A.M.N., Chamberlain D., Giles T.M. The perceived and experienced role of the nurse unit manager in supporting the wellbeing of intensive care unit nurses: An integrative literature review. Aust. Crit. Care. 2019;32:319–329. doi: 10.1016/j.aucc.2018.06.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Lee S.Y., Kim Y.Y. The effects of self-efficacy and self-directed learning readiness to self-leadership of nursing student. J. Digit. Converg. 2016;14:309–318. doi: 10.14400/JDC.2016.14.3.309. [ DOI ] [ Google Scholar ]
- 35. McGlynn K., Griffin M.Q., Donahue M., Fitzpatrick J.J. Registered nurse job satisfaction and satisfaction with the professional practice model. J. Nurs. Manag. 2012;20:260–265. doi: 10.1111/j.1365-2834.2011.01351.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Dan X., Zhang Q.M., Shi J.J., Xu S.H., Liu J.Y., Liu Y.H., Ma H.W. Improving job satisfaction of Chinese nurses: The positive effects of structural empowerment and psychological capital. TMR Integr. Nurs. 2018;2:169–177. [ Google Scholar ]
- 37. Heo M.L., Lim S.B. Development of the patient caring communication scale. Korean Soc. Nurs. Sci. 2019;49:80–91. doi: 10.4040/jkan.2019.49.1.80. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (649.3 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
You are in a modal window. Press the escape key to exit.
School of Nursing
Academic success program, strategies for problem solving.
Nursing students will be expected to have or develop strong problem-solving skills. Problem solving is centered on your ability to identify critical issues and create or identify solutions. Well-developed problem solving skills is a characteristic of a successful student. Remember, problems are a part of everyday life and your ability to resolve problems will have a positive influence on your future.
6 Steps of Problem Solving
Step 1: Identify and Define the Problem
It is not difficult to overlook the true problem in a situation and focus your attention on issues that are not relevant. This is why it is important that you look at the problem from different perspectives. This provides a broad view of the situation that allows you to weed out factors that are not important and identify the root cause of the problem.
Step 2: Analyze the Problem
Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem.
Step 3: Develop Solutions
Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
Step 4: Analyze and Select the Best Solution
List the advantages and disadvantages of each solution before deciding on a course of action. Review the advantages and disadvantages of each possible solution. Determine how the solution will resolve the problem. What are the short-term and long-term disadvantages of each solution? What are the possible short-term and long-term benefits of each solution? Which solution will help you meet your goals?
Step 5: Implement the Solution
Create a plan of action. Decide how you will move forward with your decision by determining the steps you must take to ensure that you move forward with your solution. Now, execute your plan of action.
Step 6: Evaluate the Solution
Monitor your decision. Assess the results of your solution. Are you satisfied with the results? Did your solution resolve the problem? Did it produce a new problem? Do you have to modify your solution to achieve better results? Are you closer to achieving your goal? What have you learned?
Video Modal

IMAGES
COMMENTS
Reason #1: Good Problem-Solving Skills Reflect Effective Clinical Judgement and Critical Thinking Skills The ability to quickly assess and appropriately address a variety of problems is essential in nursing. Problem-solving in nursing is the vital foundation that makes up a nurse’s clinical judgment and critical thinking skills.
Nurse problem solving. Nurse managers face challenges ranging from patient care matters to maintaining staff satisfaction. Encourage your staff to develop problem-solving nursing skills to cultivate new methods of improving patient care and to promote nurse-led innovation. Critical thinking skills are fostered throughout a nurse’s education ...
Sep 13, 2001 · The most difficult decision is deciding to tackle a problem and implement a solution, especially as it is sometimes easier to ignore its existence. Problem-solving takes time and effort, but once a problem has been addressed the nurse can feel satisfied that the issue has been resolved and is therefore less likely to re-emerge.
Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues. How to Develop and Apply Critical-Thinking Skills in Nursing ...
Sep 1, 2024 · 4. Critical Thinking & Problem Solving. Critical thinking and problem-solving are skills that every nurse should develop early in their career. Nurses often face situations where they need to make quick decisions that can affect patient outcomes.
A free flow of ideas is essential to problem-solving and decision-making because it helps prevent preconceived ideas from controlling the process. Many decisions in healthcare are arrived at by group or teams rather than by the individual, and this type of decision-making requires special skills. General steps to all decision making include:
Hospitals and nursing managers can use the hospital information system to evaluate the nursing workload, and allocate nursing human resources reasonably according to the evaluation results (H. Yang et al., 2019), so as to avoid nurses falling into the dilemma of problem solving due to long-term overloaded work.
Why are Problem Solving Skills Crucial in Nursing? Problem solving skills are fundamental in the field of Nursing because nurses regularly encounter complex and dynamic clinical situations that require quick, effective decisions. These skills help ensure patient safety, improve patient outcomes, and enhance the overall quality of care.
Nurses’ communication skills not only affected their problem-solving ability but also their understanding of patients’ conditions and nurse’s perception of professionalism. Good communication among nurses can reduce uncomfortable situations and improve interactions with patients, which can consequently enhance problem-solving [ 28 ].
Strategies for Problem Solving. Nursing students will be expected to have or develop strong problem-solving skills. Problem solving is centered on your ability to identify critical issues and create or identify solutions. Well-developed problem solving skills is a characteristic of a successful student.